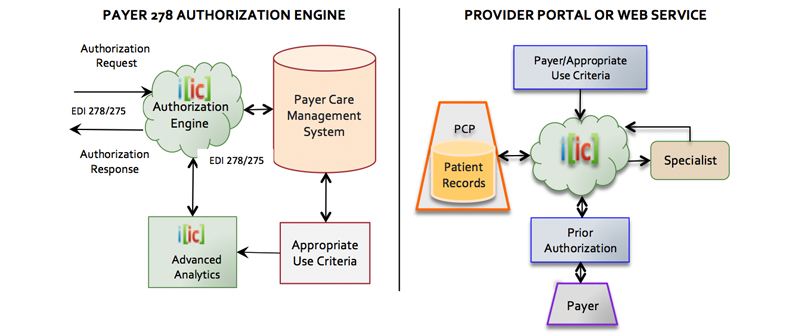
IIC is a cloud-based clinical healthcare IT company, delivering innovative and transformative solutions to automate prior authorization process via EDI 278 for both payers and providers.
PAYER PRIOR AUTHORIZATION
Prior authorization is the only effective pre-service, pre-payment method to prevent unnecessary treatment, over-utilization, and misuse. Scalability of the utilization management function based on real-time automated authorization process protects insurer payments, and enables patients to receive the most medically appropriate services based on payer policies.
IIC’s 278 Authorization Engine allows scalable utilization management and real-time adjudication based on an automated process. Payers are able to respond in real-time to the vast majority of prior authorization requests without human intervention, by automating all the payer’s policies and clinical guidelines.
PROVIDER PRIOR AUTHORIZATION
When the process is automated and real-time, prior authorization can reduce post-service denials, re-submissions, medical reviews, physician and clinical staff time, and patient rescheduling, and in turn improve patient satisfaction scores. Prior authorization is the closest assurance providers receive from payers guaranteeing payment for treatment.
The lack of automation and real-time responses causes delays in approvals, higher rate of denials, requires administrative and clinical FTEs, and delays patient treatment and outcomes. IIC’s automated EDI 278 prior authorization solution simplifies administrative processing, reduces delays, increases utilization rates, and provides a uniform workflow when submitting authorization requests to payers.
PAYER ADVANTAGES
- Comply with the ACA EDI 278 payer mandate as of Jan 1, 2016 and make EDI 278 transactions useful
- Adjudicate majority of authorization requests without human intervention
- Automate any clinical care guideline
- Scale utilization management to control over-utilization and misuse
- Configurable to meet health plans authorization criteria
- Guideline rules are editable by payer
- Allows payers to scale PA across all procedures, tests, labs, DME, etc.
- Custom analytics helps enforce evidence-based medicine
- Dramatically reduces need for medical review and re-adjudication of claims
- Hosted by IIC or easily deployed on payers’ infrastructure
PROVIDER ADVANTAGES
- PA submissions and electronic documents based on EDI 278 /275
- Submit PAs to all payers in the provider’s network from a single point of entry.
- Reduces submission time by an order of magnitude minimum.
- Uniformity and standardization of workflow within a multi-payer offering
- Reduces administrative burden, eliminates unnecessary delays, and reduces cost
- Easy to use, promoting high utilization while reducing unnecessary delays and call volumes by integrating the patient eligibility function with an electronic prior authorization request
- Enables electronic implementation to submit “Standardized Forms” for prior authorization
- Integrated with any portal or system with well-defined API or used stand-alone
