Real-Time EDI 278 Authorization Engine
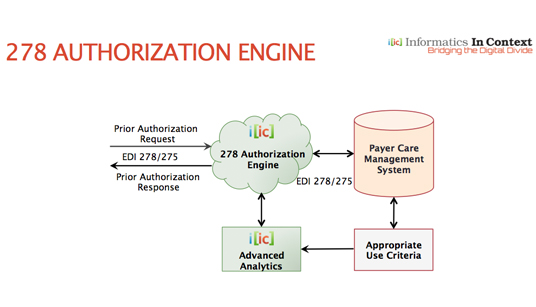
IIC’s innovative real-time 278 authorization engine is designed for health plans to automatically adjudicate all medical authorization requests using the EDI 278-275 standard. It auto processes all PA requests and provides real-time responses following the mandated criteria for those submissions. IIC’s solution is unique based on its compliance with the EDI 278-275 standard, mandated under the Affordable Care Act (ACA), and makes 278 transactions useful, not just compliant. It helps payers reduce authorization response times and transactions costs by an order of magnitude.
IIC’s 278 authorization engine handles all appropriate member data, including all subscriber files, member benefits, provider contracts, and payer policies. IIC automates all the clinical guidelines the payer uses to approve, pend, or deny PA requests and allows utilization management to scale and expand based on automating the UM process. Payers are able to respond in real-time to the vast majority of prior authorization requests without human intervention, by auto adjudicating requests using EDI 278, based on the payer’s payment policies and clinical guidelines. IIC’s authorization engine is configurable to meet all the health plans authorization criteria.
IIC’s 278 authorization engine is the first commercially available auto authorization solution for medicine based on the EDI 278-275 standard. When adjudicated correctly the first time, prior authorization prevents post-service denials, re-adjudication of claims, impacts reprocessing rates, eliminates medical review, and avoids recalculation of member liability. And it assures patients receive the most medically appropriate care based on enforcement of evidence-based medicine.
Payer Features
- Processes all prior authorization requests and responds in real-time automatically, following the mandated criteria for those submissions
- Automated prior authorization responses are based on the payers’ specific policies and clinical guidelines. Clinical guidelines and rules are editable by the payer as they change.
- 278 authorization engine is easily configurable to handle all subscriber data, as well as the payer’s payment policies, payer contracts, member benefits, and clinical guidelines
- Payers continue to use their existing workflow without disruption
- Advanced analytics are used to detect provider trends and patterns, along with helping enforce evidence-based medicine
- Analytic triggers can be applied to fraud alerts, provider submission patterns, procedure selection patterns, and much more
Payer Benefits
- IIC’s solution addresses the manual nature of PA adjudication using a real-time automated process
- Automate any clinical guideline (i.e. CMS, MCG, InterQual, ODG, Custom)
- Adjudicate the vast majority of PA requests automatically without human intervention
- Scale and expand utilization management to control over-utilization, fraud, waste, and abuse
- Dramatically reduce the need for medical review, appeals, denials, and re-adjudication of claims
- Make 278 transactions functional and comply with the ACA mandate of Jan 1, 2016
- Payer realize an order of magnitude savings in admin processing time and cost, along with a dramatic increase in workflow efficiency and administrative simplification.
- Automated improves timelines of overall claims adjudication
- Value of prepayments ties authorization claim to approval code, avoiding the “pay and chase” scenario (i.e. post-payment reviews and denials where payment has already been remitted to the provider).
- By significantly lowering internal costs, payers can redirect limited resources without increasing budget
- Advanced analytics helps enforce evidence-based medicine
- Helps payer maintain member satisfaction ratings, which impacts programs such as Medicare Five Star Quality Rating, etc.
